3 supplements for fatty liver disease: what the research actually shows
Fish oil, vitamin D, and carnitine may help fatty liver disease. Here's what the clinical evidence says about each supplement and who might benefit.
Fatty liver disease has become remarkably common. About one in three adults in Western countries has some degree of fat accumulation in their liver, and the numbers are climbing. If you’ve been diagnosed with non-alcoholic fatty liver disease (NAFLD), you’ve probably been told to lose weight, exercise more, and eat better. That’s genuinely good advice. Weight loss remains the most effective intervention we have.
But you might be wondering whether supplements can help. I’ve gone through the clinical research on three that show up frequently in discussions about fatty liver: fish oil, vitamin D, and carnitine. Here’s what the evidence actually shows.
Understanding fatty liver disease first
Before getting into supplements, it helps to understand what’s going on in the liver.
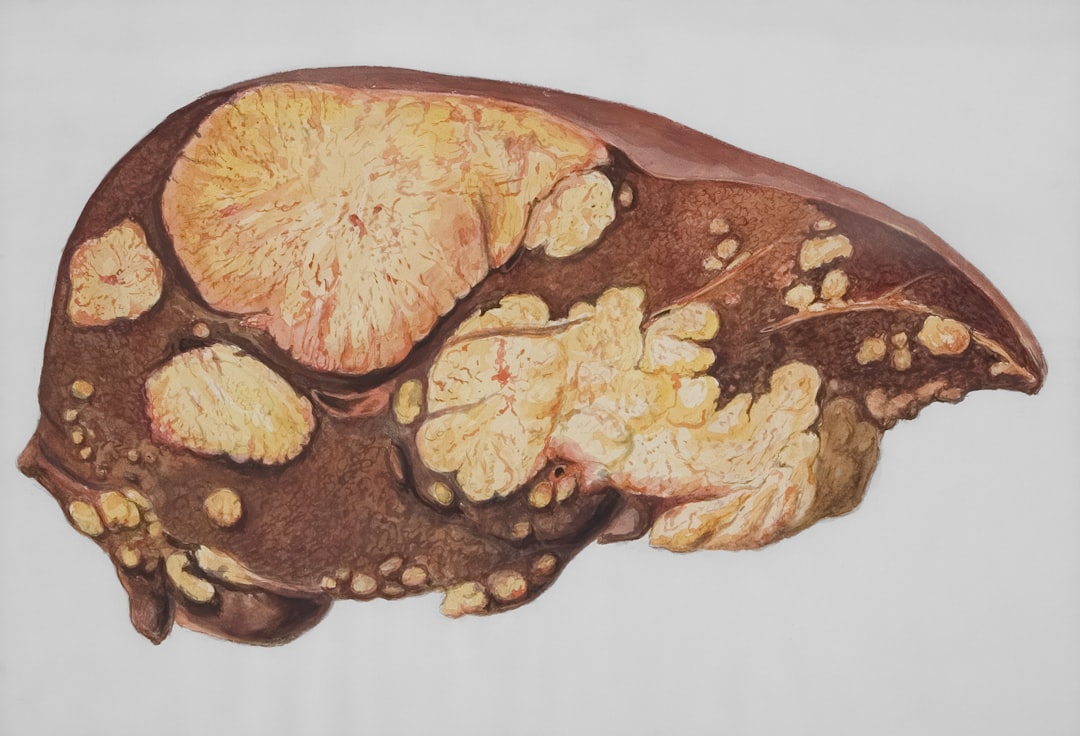
Non-alcoholic fatty liver disease occurs when fat accumulates in liver cells without significant alcohol consumption. The NHS defines it as fat making up more than 5-10% of your liver’s weight [1]. Most people with fatty liver have no symptoms and discover it incidentally through blood tests or imaging done for other reasons.
The concerning part isn’t the fat itself. It’s what can happen next. Some people progress to non-alcoholic steatohepatitis (NASH), where the liver becomes inflamed and scarred. From there, a smaller number develop cirrhosis or liver cancer. The progression isn’t inevitable, but it’s worth taking seriously.
Who gets fatty liver? The condition correlates strongly with diabetes, obesity, high triglycerides, and metabolic syndrome. If you have several of these conditions together, the likelihood of fatty liver increases substantially. Men develop it roughly twice as often as women, though the gap narrows after menopause [2].
1. Fish oil (omega-3 fatty acids)
Fish oil is the supplement with the most research behind it for fatty liver disease. The omega-3 fatty acids EPA and DHA, found in oily fish and fish oil supplements, have been studied in multiple clinical trials.
What the evidence shows
A 2016 Cochrane review examined 18 randomised controlled trials involving 1,424 participants with NAFLD [3]. The researchers found that omega-3 supplementation reduced liver fat content, though they noted the quality of evidence was low to moderate. More recent meta-analyses have reached similar conclusions.
A 2020 systematic review pooling data from 22 studies found that omega-3 supplementation significantly reduced liver fat, improved liver enzyme levels (ALT and AST), and lowered triglycerides [4]. The effects on inflammation markers were more modest.
How might omega-3s help? Several mechanisms have been proposed. Fish oil appears to activate receptors (PPAR-alpha) that promote fat breakdown in the liver, reduce the production of new fat, improve insulin sensitivity, and decrease inflammation [5]. Animal studies support these mechanisms, though translating animal findings to humans is always uncertain.
My honest assessment
The research is reasonably consistent. Fish oil does appear to reduce liver fat in most trials. However, the effect sizes are modest, and we don’t have good long-term data showing that this translates to fewer people developing cirrhosis or liver cancer.
What gives me pause is that the clinical improvement often doesn’t match the reduction in liver fat. People may have less fat in their liver on imaging, but their liver function tests don’t always improve proportionally. That suggests we might be measuring a surrogate marker rather than something that directly predicts better outcomes.
If you already eat oily fish (salmon, mackerel, sardines) a few times per week, you’re probably getting adequate omega-3s. Supplements make more sense for people who don’t eat much fish. Typical doses in studies were 2-4 grams of combined EPA and DHA daily.
Read more about fish oil in our detailed article on the benefits and side effects of fish oil.
2. Vitamin D
The connection between vitamin D and fatty liver has been a hot research topic. People with NAFLD consistently have lower vitamin D levels than those without the condition. But correlation isn’t causation, and disentangling this relationship has proved tricky.
The observational evidence
Multiple studies have found that people with NAFLD have lower blood vitamin D concentrations than matched controls. A meta-analysis combining six studies found that NAFLD patients were 26% more likely to have severe vitamin D deficiency (below 20 ng/mL) [6]. Similar patterns appear in children with fatty liver.
Why might vitamin D be related to fatty liver? Vitamin D receptors exist throughout the liver, and the vitamin appears to affect insulin sensitivity, inflammation, and fat metabolism. Vitamin D deficiency also correlates with obesity and metabolic syndrome, which themselves cause fatty liver. Teasing apart these overlapping relationships is difficult [7].
The intervention trials
Here’s where things get more complicated. Observational studies suggested vitamin D might help, but the randomised controlled trials have been mixed.
A 2019 meta-analysis of 11 trials found that vitamin D supplementation improved some liver enzyme levels but didn’t significantly reduce liver fat on imaging [8]. A more recent 2021 meta-analysis found modest improvements in ALT levels and insulin resistance, but again, the effects on liver fat itself were inconsistent [9].
The trials have used varying doses (from 2,000 IU to 50,000 IU weekly), different vitamin D forms, and different durations. This heterogeneity makes drawing firm conclusions difficult.
My honest assessment
I think vitamin D supplementation makes sense if you’re actually deficient, which many people are. The Mayo Clinic suggests that adults need 600-800 IU daily, and many with fatty liver fall short [10]. But I wouldn’t expect vitamin D alone to reverse fatty liver disease.
If your blood vitamin D level is below 20 ng/mL, correcting that deficiency is worthwhile for reasons beyond liver health (bone health, immune function, possibly cardiovascular health). Whether supplementation helps people with adequate vitamin D levels is less clear.
3. Carnitine
Carnitine is less well-known than fish oil or vitamin D, but it has a logical connection to fatty liver. This amino acid derivative helps transport fatty acids into mitochondria, where they’re burned for energy. In theory, if carnitine helps the liver burn fat more efficiently, less fat should accumulate.
What the research shows
The evidence base for carnitine is smaller than for fish oil, but what exists is reasonably encouraging.
A 2014 randomised controlled trial gave 74 NAFLD patients either 2 grams of L-carnitine daily or placebo for six months [11]. The carnitine group showed greater reductions in liver enzyme levels, inflammatory markers, and blood sugar. Ultrasound showed improvements in liver appearance as well.
A 2019 meta-analysis pooled data from several trials and found that L-carnitine supplementation significantly reduced ALT, AST, and fasting blood glucose in NAFLD patients [12]. The improvements in liver enzymes were more consistent than those seen with vitamin D.
The proposed mechanism involves mitochondrial function. In NAFLD, mitochondria often work poorly, leading to increased oxidative stress and inflammation. Carnitine supplementation may help restore normal mitochondrial function, allowing the liver to process fats more efficiently [13].
My honest assessment
The carnitine research is promising but limited. Most trials have been small (under 100 participants) and relatively short (three to six months). We don’t have data on whether carnitine prevents progression to NASH or cirrhosis.
I’d consider carnitine a reasonable option to try, particularly if you’ve already addressed diet and exercise but want additional support. The typical dose in studies was 2 grams daily. Side effects are generally mild (occasional nausea or fishy body odour at high doses).
What the research doesn’t support
It’s worth mentioning a few supplements that are sometimes promoted for fatty liver but lack good evidence:
Milk thistle (silymarin) has a long history as a liver tonic, but trials in NAFLD have been inconsistent. Some show modest benefit, others show none. The quality of milk thistle supplements also varies considerably.
Turmeric/curcumin has anti-inflammatory properties in laboratory studies, but human trials in NAFLD have been mixed. Read more in our curcumin article.
Probiotics may have some effect on liver enzymes, but the evidence is preliminary. Different probiotic strains have different effects, making generalisation difficult.
What actually works for fatty liver
Supplements may help at the margins, but the interventions with the strongest evidence are lifestyle changes:
Weight loss is the most effective treatment. Losing 7-10% of body weight typically produces meaningful reductions in liver fat and inflammation. The NHS recommends gradual weight loss through sustainable dietary changes rather than crash diets [1].
Exercise improves fatty liver even without weight loss. Both aerobic exercise and resistance training appear beneficial. The mechanism may involve improved insulin sensitivity and direct effects on liver metabolism.
Dietary changes matter beyond calories. Mediterranean-style diets (emphasising vegetables, olive oil, fish, and nuts while limiting processed foods and sugar) show particular benefit in NAFLD. Reducing sugar-sweetened beverages and fructose appears especially important.
Limiting alcohol makes sense even in “non-alcoholic” fatty liver. The liver doesn’t need additional stress while trying to recover.
Safety considerations
If you’re considering supplements for fatty liver, a few cautions:
Fish oil can increase bleeding risk, particularly at high doses or combined with aspirin or other blood thinners. If you’re scheduled for surgery or have a bleeding disorder, discuss this with your doctor.
Vitamin D toxicity is possible with very high doses over long periods. Stick to reasonable supplementation (1,000-4,000 IU daily) unless you have documented severe deficiency requiring higher doses under medical supervision.
Carnitine can interact with thyroid medications and anticonvulsants. It may also worsen hypothyroidism in some people.
If you have diabetic bladder dysfunction or are managing diabetes alongside fatty liver, coordinate any supplement use with your healthcare team, as both conditions share underlying metabolic issues.
The bottom line
No supplement will cure fatty liver disease. That’s the reality. The most effective intervention remains weight loss through diet and exercise.
That said, fish oil has the most consistent evidence for reducing liver fat. Vitamin D supplementation makes sense if you’re deficient. Carnitine shows promise but needs more research.
I wouldn’t prioritise supplements over lifestyle changes. But if you’ve already committed to better diet and regular exercise, adding one of these supplements might provide additional modest benefit. Talk to your doctor about which, if any, makes sense for your situation.
Related reading
- Fish oil: benefits, side effects, and contraindications
- Supplements for diabetes: what the research shows
- Resveratrol: benefits, side effects, and contraindications
References
-
NHS. Non-alcoholic fatty liver disease (NAFLD). https://www.nhs.uk/conditions/non-alcoholic-fatty-liver-disease/
-
Lonardo A, Nascimbeni F, Ballestri S, et al. Sex differences in nonalcoholic fatty liver disease: state of the art and identification of research gaps. Hepatology. 2019;70(4):1457-1469. PMID: 30924946
-
Parker HM, Johnson NA, Burdon CA, et al. Omega-3 supplementation and non-alcoholic fatty liver disease: a systematic review and meta-analysis. J Hepatol. 2012;56(4):944-951. PMID: 22023985
-
Yan JH, Guan BJ, Gao HY, Peng XE. Omega-3 polyunsaturated fatty acid supplementation and non-alcoholic fatty liver disease: A meta-analysis of randomized controlled trials. Medicine (Baltimore). 2018;97(37):e12271. PMID: 30212963
-
Jump DB, Depner CM, Tripathy S, Lytle KA. Potential for dietary ω-3 fatty acids to prevent nonalcoholic fatty liver disease and reduce the risk of primary liver cancer. Adv Nutr. 2015;6(6):694-702. PMID: 26567195
-
Eliades M, Spyrou E, Agrawal N, et al. Meta-analysis: vitamin D and non-alcoholic fatty liver disease. Aliment Pharmacol Ther. 2013;38(3):246-254. PMID: 23786213
-
Targher G, Bertolini L, Scala L, et al. Associations between serum 25-hydroxyvitamin D3 concentrations and liver histology in patients with non-alcoholic fatty liver disease. Nutr Metab Cardiovasc Dis. 2007;17(7):517-524. PMID: 16928437
-
Guo XF, Wang C, Yang T, et al. Vitamin D and non-alcoholic fatty liver disease: a meta-analysis of randomized controlled trials. Food Funct. 2020;11(9):7389-7399. PMID: 32797115
-
Pramono A, Jocken JWE, Goossens GH, Blaak EE. Effects of vitamin D supplementation on insulin sensitivity: a systematic review and meta-analysis. Diabetes Care. 2020;43(7):1659-1669. PMID: 32540990
-
Mayo Clinic. Vitamin D. https://www.mayoclinic.org/drugs-supplements-vitamin-d/art-20363792
-
Malaguarnera M, Gargante MP, Russo C, et al. L-carnitine supplementation to diet: a new tool in treatment of nonalcoholic steatohepatitis—a randomized and controlled clinical trial. Am J Gastroenterol. 2010;105(6):1338-1345. PMID: 20068559
-
Abolfathi M, Mohd-Yusof BN, Hanipah ZN, et al. The effects of carnitine supplementation on clinical characteristics of patients with non-alcoholic fatty liver disease: A systematic review and meta-analysis of randomized controlled trials. Complement Ther Med. 2020;48:102273. PMID: 31987222
-
Savic D, Hodson L, Neubauer S, Pavlides M. The importance of the fatty acid transporter L-carnitine in non-alcoholic fatty liver disease (NAFLD). Nutrients. 2020;12(8):2178. PMID: 32708025
Medical Disclaimer: The information provided is for educational purposes only and should not be considered as medical advice. Always consult with a qualified healthcare professional before making any changes to your diet, supplement regimen, or treatment plan.