Cystistat: Sodium Hyaluronate Bladder Instillation for Interstitial Cystitis
Cystistat delivers sodium hyaluronate directly into the bladder to treat interstitial cystitis. Learn how it works, what research shows, and what to expect.
What Is Cystistat?
Cystistat is a medical device containing sodium hyaluronate (the sodium salt of hyaluronic acid) that is instilled directly into the bladder to treat interstitial cystitis (IC) and painful bladder syndrome (PBS). It is one of several intravesical (inside-the-bladder) therapies available for patients who have not responded adequately to oral medications.
The product comes pre-packaged as a sterile solution ready for instillation via a catheter. Unlike oral supplements, which must survive digestion and travel through the bloodstream, Cystistat delivers the active ingredient directly to the bladder lining where it is needed.
I should be clear from the start: this is not a cure for IC or PBS. It is a symptom management treatment that works by temporarily replenishing a protective layer on the bladder wall. Some patients experience significant relief, while others notice little difference. As with most IC treatments, individual responses vary considerably.
The Science Behind Sodium Hyaluronate
To understand how Cystistat works, you need to know a bit about the bladder’s natural protective mechanisms.
The GAG Layer
The inner surface of a healthy bladder is coated with a layer of glycosaminoglycans (GAGs). This layer includes substances like hyaluronic acid, chondroitin sulphate, and heparan sulphate. Together, they form a protective barrier that prevents urine components from irritating the underlying bladder tissue.
In many patients with IC/PBS, researchers believe this GAG layer is deficient or damaged 1. Without adequate protection, toxic substances in urine can penetrate the bladder wall and trigger inflammation and pain—the urgency, frequency, and discomfort that make IC so difficult to live with.
How Sodium Hyaluronate Helps
Sodium hyaluronate is a naturally occurring molecule found throughout the body, including in joint fluid, the eye, and the bladder lining itself. When instilled into the bladder, it temporarily coats the damaged areas and acts as a substitute for the missing GAG layer.
The treatment does not fix the underlying problem permanently. Instead, it provides a temporary protective barrier that may allow the bladder tissue to heal and reduce symptom severity. This is why repeated treatments are typically necessary.
My understanding: Think of it like applying a protective dressing to an open wound. The dressing does not heal the wound directly, but it creates conditions that allow healing to occur while reducing pain in the meantime.
What Does the Clinical Evidence Show?
The evidence base for sodium hyaluronate bladder instillations is reasonably solid, though I would not call it overwhelming. Most studies are relatively small, and head-to-head comparisons with other treatments are limited.
Early Clinical Studies
One of the foundational studies involved 20 patients with IC who received weekly sodium hyaluronate instillations for four weeks. At three-month follow-up, 12 patients (60%) showed clear improvement, with reduced pain and increased bladder capacity 2.
Another study followed 121 patients receiving sodium hyaluronate therapy. At five-year follow-up, 65% of responders maintained their improvement with periodic top-up treatments. The average treatment interval extended from monthly to once every four months as patients stabilised 3.
Comparative Studies
A randomised controlled trial compared sodium hyaluronate with DMSO (dimethyl sulfoxide), an older intravesical treatment with a stronger evidence base but notable side effects. After six weeks of treatment, 85% of the sodium hyaluronate group reported improvement compared to 61% in the DMSO group, though the difference did not reach statistical significance in this relatively small study 4.
Combination Approaches
Some clinicians combine sodium hyaluronate with other agents. A study examining hyaluronic acid plus chondroitin sulphate in 126 IC patients found that 87% experienced clear symptom improvement at 12 weeks, with 62% maintaining this improvement at 12 months 5.
My honest assessment: The evidence suggests sodium hyaluronate helps a meaningful proportion of IC/PBS patients, though response rates vary across studies (roughly 50-85% showing some improvement). It appears to be well tolerated with few side effects, which is a genuine advantage over some alternatives. However, the studies are generally small, and long-term data are limited.
How Treatment Works in Practice
Understanding what to expect from Cystistat treatment can help you prepare and set realistic expectations.
The Instillation Procedure
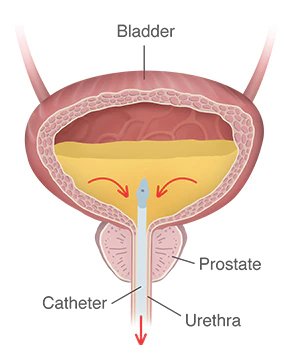
Cystistat is administered by a healthcare professional, typically a urologist or specialist nurse, in an outpatient clinic setting. The procedure involves:
- A thin catheter is inserted into the bladder through the urethra
- The sterile Cystistat solution is slowly instilled into the bladder
- The catheter is removed
- You are asked to retain the solution for as long as comfortable, ideally 30-60 minutes
- You then urinate to empty the bladder
The procedure itself takes only a few minutes, though you should allow time for the retention period. Most patients tolerate it well, though catheter insertion can be uncomfortable for some people.
Treatment Schedule
The typical protocol has two phases. During weeks 1-4, you receive weekly instillations to build up the protective coating. After that, treatments are spaced further apart based on how you respond. Many patients move to monthly instillations initially, then extend the interval to every 6, 8, or even 12 weeks if symptoms stay controlled.
One thing worth knowing: do not be discouraged if you do not notice improvement straight away. Some patients need five or six instillations before experiencing real symptom relief. Response tends to develop gradually rather than dramatically after a single treatment.
Duration of Treatment
There is no set endpoint for Cystistat therapy. Some patients remain on maintenance treatment indefinitely, while others are able to discontinue treatment after a period of stability. If symptoms return after stopping, treatment can be resumed.
The goal is to find the minimum treatment frequency that maintains adequate symptom control for each individual patient.
Side Effects and Safety
Cystistat has a good safety profile. Because sodium hyaluronate occurs naturally in the body and the treatment stays local rather than circulating systemically, serious adverse reactions are rare.
Common Experiences
The most frequently reported issue is temporary discomfort related to the catheterisation procedure itself rather than the sodium hyaluronate solution:
- Mild burning or stinging during catheter insertion
- Brief urgency or discomfort immediately after instillation
- Occasional spotting of blood in urine following the procedure
These effects typically resolve within a day or two.
Uncommon Reactions
Rarely, some patients experience a temporary flare in symptoms shortly after instillation. This usually settles within 24-48 hours. If you experience severe or persistent symptoms after treatment, contact your healthcare team.
Who Should Not Use Cystistat
Cystistat is contraindicated in patients with:
- Active urinary tract infection (treatment should be delayed until infection resolves)
- Known hypersensitivity to hyaluronic acid or any component of the product
- Bladder injury or recent bladder surgery where instillation might cause complications
There are no known significant drug interactions, and the treatment can generally be used alongside other IC medications.
How Cystistat Compares to Other Treatments
If you are considering Cystistat, you may be wondering how it stacks up against alternatives.
Versus Oral Medications
Oral treatments like pentosan polysulfate sodium (Elmiron) work systemically and take months to show effect. Cystistat delivers treatment directly to the bladder and may show results more quickly in responsive patients. However, oral medications do not require clinic visits for administration.
Versus DMSO
DMSO has a longer track record and is the only FDA-approved intravesical treatment for IC. However, it can cause a garlic-like taste and odour, temporary bladder irritation, and requires eye examinations during prolonged use due to potential lens changes. Sodium hyaluronate generally has fewer side effects.
Versus Alkalinised Lidocaine
Treatments like Cystilieve work by anaesthetising the bladder rather than replenishing the GAG layer. They may provide faster pain relief but address symptoms differently. Some protocols combine both approaches.
Versus Heparin
Intravesical heparin is another GAG-layer replenishment therapy with similar goals to sodium hyaluronate. Some studies suggest combination therapy (heparin plus hyaluronic acid) may be more effective than either alone.
Worth noting: IC/PBS treatment often involves trial and error. What works brilliantly for one patient may be ineffective for another. Many patients try multiple approaches before finding their optimal management strategy.
Obtaining Treatment
Cystistat is classified as a medical device rather than a pharmaceutical drug, which affects how it is regulated and supplied. It requires administration by qualified healthcare professionals, meaning you cannot simply purchase it and use it at home.
In the UK
Cystistat is available through NHS urology departments for patients meeting clinical criteria. Availability may vary by region and local commissioning decisions. Private treatment is also an option for those who prefer it or face NHS waiting times.
The Referral Process
To access Cystistat, you typically need:
- A diagnosis of IC/PBS from a urologist
- Documentation that other treatments have been tried without adequate relief
- Assessment by a specialist who confirms intravesical therapy is appropriate
Your GP can refer you to a urologist if you are experiencing chronic bladder symptoms that have not responded to initial treatments.
Practical Tips for Patients
Based on clinical experience and patient feedback, here are some practical suggestions.
Empty your bladder just before the procedure. This allows maximum contact time between the solution and your bladder lining.
During the retention period, some patients find it helpful to change positions—sitting, lying on each side, lying on their back—to help the solution coat all areas of the bladder.
After treatment, drink normally but do not overdo fluid intake in the first few hours. Excessive drinking will dilute and flush out the treatment faster.
Keep a bladder diary noting symptoms, urgency episodes, and pain levels. This helps you and your clinician figure out whether the treatment is actually working and fine-tune your schedule. Without tracking, it is hard to tell gradual improvement from wishful thinking.
Questions to Ask Your Urologist
If you are considering Cystistat, here are some questions worth discussing:
- How many of your patients have tried sodium hyaluronate, and what have their experiences been?
- What symptoms are most likely to respond to this treatment?
- How will we know if the treatment is working, and how long should we trial it before reassessing?
- What happens if this treatment is not effective for me?
- Are there other intravesical options I should consider first or in combination?
Is Cystistat worth trying?
If I had IC/PBS and oral medications were not cutting it, I would consider Cystistat. The evidence suggests it helps roughly half to three-quarters of patients who try it, and it has fewer side effects than DMSO. That counts for something.
But I would go in with clear expectations. This is not a cure. You will probably need repeated treatments, possibly indefinitely. You have to make regular clinic visits for catheterisation, which some people find uncomfortable or inconvenient. And there is no guarantee it will work for you specifically.
For patients who have bounced off other treatments or cannot tolerate systemic medications, Cystistat is a reasonable option to discuss with your urologist. Just give it a proper trial—at least five or six instillations—before deciding whether it is helping.
References
-
Parsons CL. The role of the urinary epithelium in the pathogenesis of interstitial cystitis/prostatitis/urethritis. Urology. 2007;69(4 Suppl):9-16. PubMed
-
Morales A, Emerson L, Nickel JC, Lundie M. Intravesical hyaluronic acid in the treatment of refractory interstitial cystitis. J Urol. 1996;156(1):45-48. PubMed
-
Kallestrup EB, Jorgensen SS, Nordling J, Hald T. Treatment of interstitial cystitis with Cystistat: a hyaluronic acid product. Scand J Urol Nephrol. 2005;39(2):143-147. PubMed
-
Daha LK, Riedl CR, Hohlbrugger G, Knoll M, Engelhardt PF, Pflüger H. Comparative assessment of maximal bladder capacity, 0.9% NaCl versus 0.2 M Kcl, for the diagnosis of interstitial cystitis: a prospective controlled study. J Urol. 2003;170(3):807-809. PubMed
-
Cervigni M, Natale F, Nasta L, Padoa A, Voi RL, Porru D. A combined intravesical therapy with hyaluronic acid and chondroitin for refractory painful bladder syndrome/interstitial cystitis. Int Urogynecol J. 2012;23(9):1193-1199. PubMed
Medical Disclaimer: The information provided is for educational purposes only and should not be considered as medical advice. Always consult with a qualified healthcare professional before making any changes to your diet, supplement regimen, or treatment plan.