Fecal Transplant for Recurrent UTIs: What Research Shows
Can a fecal transplant prevent recurrent UTIs? We review the latest 2025 research on FMT for UTI prevention, including a reported 93% reduction in infections.
If you’ve been caught in the cycle of recurrent UTIs and repeated antibiotics, you’re not alone. About 20-30% of women who get a UTI will get another one, and each round of antibiotics can make the next infection more likely and harder to treat. It’s a frustrating loop that drives millions of people to search for alternatives.
One of the most unexpected alternatives to emerge from recent research is the fecal microbiota transplant, or FMT. Yes, transferring healthy gut bacteria from a donor into a patient’s digestive system. The idea sounds strange, but the science behind it is solid, and the early results for recurrent UTIs are striking. A 2025 Cleveland Clinic study reported a 93% reduction in UTI frequency after fecal transplant 1.
This article walks through the research on fecal transplant for recurrent UTIs, what we know, what we don’t, and whether this could eventually become a real option for patients.
The Problem: Why Recurrent UTIs Keep Coming Back
Urinary tract infections affect an estimated 150 million people worldwide each year. More than 60% of women will experience at least one UTI in their lifetime, and among those, 20-30% develop recurrent infections, typically defined as two or more UTIs within six months or three within a year.
The standard treatment is antibiotics. But here’s the catch: antibiotics kill bacteria in the bladder, but the bacteria that caused the infection usually came from the gut in the first place. The E. coli living in your intestines migrate to the urinary tract through what researchers call the gut-bladder axis. Antibiotics clear the bladder infection but leave the gut reservoir intact. Worse, they damage your protective gut bacteria in the process.
A landmark 2022 study published in Nature Microbiology by Worby and colleagues tracked 31 women over a year with monthly stool, urine, and blood samples. Women with recurrent UTIs had significantly less diverse gut bacteria and were missing key butyrate-producing species that help keep inflammation in check 2. Their gut microbiomes resembled those of people with inflammatory conditions.
In other words, the very treatment for UTIs may be making people more vulnerable to the next one.
How Your Gut Causes Bladder Infections
The connection between gut bacteria and bladder infections is not a theory anymore. It’s been documented at the strain level.
A 2019 study in Nature Communications analyzed 510 stool samples from 168 kidney transplant recipients. When UTI-causing bacteria like E. coli reached just 1% of total gut bacteria, the risk of developing a bladder infection increased significantly. Genetic sequencing confirmed that the bacteria found in patients’ urine were the same strains present in their gut 3.
The largest study on this topic came from a CDC Prevention Epicenters collaboration published in eClinicalMedicine (a Lancet journal) in 2024. Analyzing 644 stool samples from 125 patients, researchers found that recurrent UTI patients had distinctly different gut bacteria from healthy people, with elevated levels of antibiotic-resistance genes 4.
The mechanism works like this: UTI-causing E. coli live in your intestines. They migrate to the vaginal area, then up the urethra into the bladder. Antibiotics wipe out the bladder infection but also destroy beneficial gut bacteria that were keeping the E. coli population under control. Without that competition, E. coli bounces back and eventually causes another infection.
This is why researchers started asking: what if we could fix the gut instead of just treating the bladder?
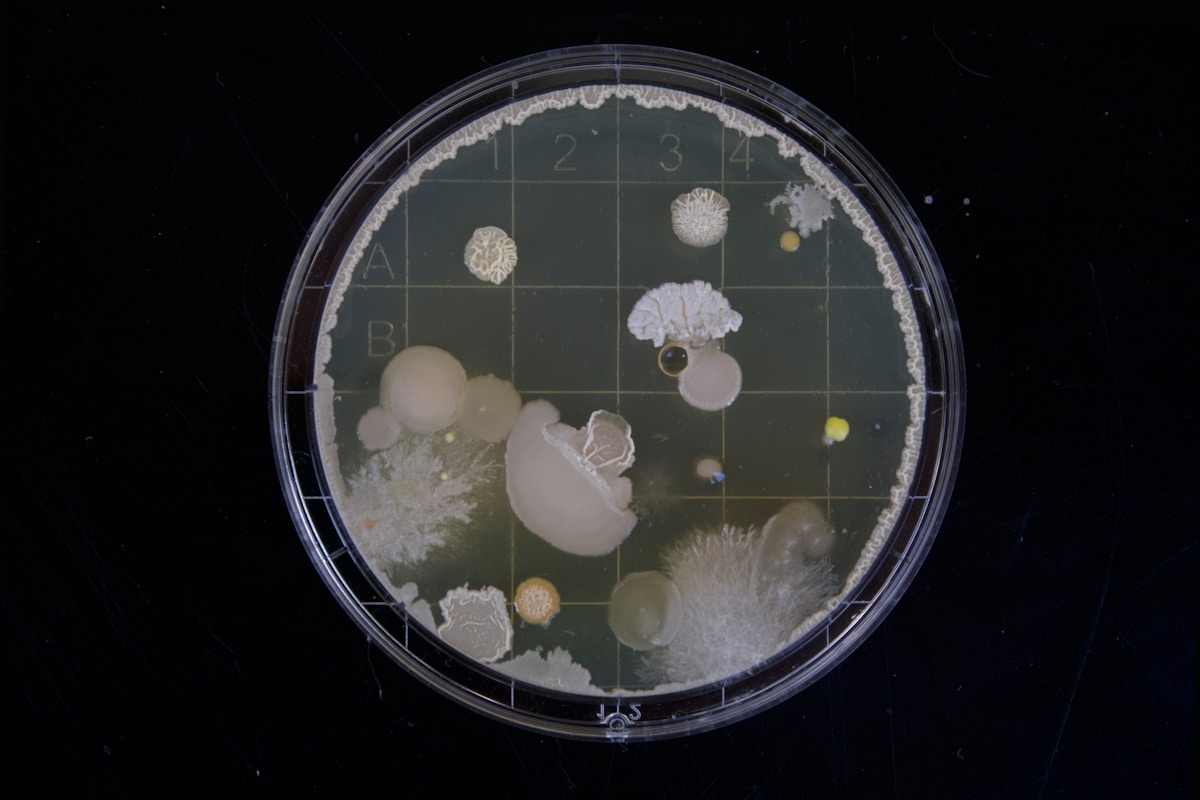
What Is a Fecal Microbiota Transplant?
A fecal microbiota transplant takes healthy gut bacteria from a carefully screened donor and transfers them into a patient’s digestive system. The goal is to restore a diverse, balanced gut microbiome.
FMT is already FDA-approved for one condition: recurrent Clostridioides difficile (C. diff) infection, where it works remarkably well. Two products, Rebyota and Vowst, are approved for this use.
For UTIs, FMT is still investigational. It’s not something you can request from your doctor as a standard treatment. But the rationale is straightforward: if UTI-causing bacteria originate in the gut, and a damaged gut microbiome allows those bacteria to thrive, then restoring healthy gut bacteria should reduce the reservoir of pathogens available to cause infections.
FMT can be delivered several ways:
- Colonoscopy (direct delivery to the colon)
- Oral capsules containing freeze-dried donor material
- Enema
- Nasojejunal tube (less common)
The oral capsule approach is gaining traction in recent UTI research because it’s the least invasive and most scalable.
The Evidence: What Clinical Studies Show
The clinical data on fecal transplant for recurrent UTIs is still early stage, with small sample sizes across all studies. But the consistency of results across independent research groups is worth paying attention to.
2025 Cleveland Clinic Study (Strongest Results)
Jeong and colleagues at the Cleveland Clinic published results in Urology showing the most dramatic outcomes yet. Among 11 patients with recurrent UTIs who received FMT (originally for C. difficile), average UTI frequency dropped from 3.7 infections over two years to just 0.27. That’s a 93% reduction. No patient had recurrent UTIs during follow-up, with a median time to any UTI recurrence of 19.6 months 1.
My take: these numbers are impressive, but the study was retrospective (looking back at records) and the patients received FMT for C. diff, not specifically for UTIs. The UTI reduction was an observed secondary benefit. That said, it lines up with other findings.
2025 Proof-of-Concept Trial (Postmenopausal Women)
A European team designed the first study specifically testing FMT for UTI prevention. They treated 22 postmenopausal women with oral rifaximin (to clear some existing gut bacteria) followed by freeze-dried FMT capsules. UTI episodes dropped by 68%, from an average of 5 per patient to 1.6. Roughly 41% of participants had multidrug-resistant bacteria before treatment. In 3 out of 4 cases with ESBL-producing Klebsiella, the resistant bacteria were completely eliminated from the gut. Post-FMT recurrences were caused by antibiotic-susceptible bacteria, not resistant ones 5.
This last point is particularly interesting. FMT didn’t just reduce UTI frequency. It reversed antibiotic resistance.
2020 Prospective Case Series (First Direct UTI Trial)
Jeney and colleagues at UC Irvine enrolled 11 women (10 completed treatment) in the first prospective study of FMT specifically for refractory recurrent UTIs. Median UTIs dropped from 3 to 1 over six months. Four women no longer met the criteria for recurrent UTI. Three had zero infections after treatment. Before FMT, 6 women carried ESBL-producing bacteria; this dropped to just 1 at three months. Gut microbiome diversity increased significantly 6.
The study didn’t reach statistical significance (p=0.055), likely due to the small sample size. But the trend was clear.
2017 Mayo Clinic Study (First Published Evidence)
The first published evidence came from Tariq and colleagues at the Mayo Clinic. Among 8 patients who received FMT for C. diff, those with recurrent UTIs saw their infections drop from a median of 4 per year to 1 per year, a 75% reduction. Antibiotic susceptibility profiles of UTI-causing organisms also improved 7.
2023 Case Report (18 Months Infection-Free)
A Houston Methodist case report described a patient with an ileal conduit and urostomy who suffered recurrent ESBL-producing Klebsiella pneumoniae UTIs. After oral freeze-dried FMT capsules, the patient went 18 months without a single infection. The resistant bacteria disappeared from follow-up cultures entirely 8.
2025 Kidney Transplant Study
Hu and colleagues studied 18 kidney transplant recipients who received FMT. Urinary infection markers dropped significantly (p<0.001), and gut bacteria shifted toward beneficial butyrate-producing species like Faecalibacterium and Roseburia, while the uropathogen Enterococcus decreased 9.
Economic Impact
A 2023 Danish study calculated the cost-effectiveness of FMT for UTI patients. Among 5 patients, median UTIs dropped from 4 to zero after treatment. Hospital admission days fell by 87%, and monthly healthcare costs dropped by 79% 10.
The Antibiotic Resistance Angle
One of the most compelling aspects of this research goes beyond just preventing UTIs. It’s about antibiotic resistance.
Antibiotic-resistant urinary tract infections are a growing crisis. Recent data from CIDRAP shows that 57% of first-time UTIs are already resistant to at least one antibiotic class. By the sixth infection, resistance climbs to 65%, and 20% of patients harbor bacteria resistant to three or more drug classes.
Fluoroquinolone-resistant E. coli has increased from 4% to 12% in North America over the past decade. In parts of Asia, resistance rates exceed 40%.
Several FMT studies have shown that restoring a healthy gut microbiome doesn’t just reduce UTI frequency. It actually reverses resistance patterns. The 2025 proof-of-concept trial found that post-FMT UTIs were caused by drug-susceptible bacteria, not the resistant strains that were there before 5. The 2020 UC Irvine trial showed ESBL-producing bacteria disappearing from patients’ guts 6.
The theory is that a diverse, healthy microbiome outcompetes resistant bacteria for resources. When gut diversity collapses (usually from antibiotics), resistant strains have less competition and multiply.
Limitations and What We Don’t Know Yet
I need to be straightforward about the limitations, because the hype around FMT can run ahead of the evidence.
Small sample sizes. The largest direct FMT-for-UTI study included 22 patients. Most had fewer than 15. We need trials with hundreds of participants to confirm these results hold up at scale.
No randomized controlled trials yet. Most studies are retrospective analyses, case series, or proof-of-concept designs. The gold standard, double-blind randomized controlled trials, hasn’t been completed for this specific use.
Unknown long-term effects. Follow-up periods range from 6 to 20 months. We don’t know if the benefits persist for years, or whether patients need repeat treatments.
Donor variability. Not all donor microbiomes are equal. Research in C. diff has shown that donor selection significantly affects outcomes, and we don’t yet know which donor characteristics matter most for UTI prevention.
Regulatory status. FMT for UTIs is not FDA-approved and remains investigational. The only way to access it currently is through clinical trials or compassionate-use programs.
There is at least one active clinical trial registered on ClinicalTrials.gov (NCT03367910) specifically studying FMT for UTIs caused by multidrug-resistant organisms.
Other Emerging Gut-Based Approaches
FMT isn’t the only research avenue targeting the gut-bladder connection. Several other approaches are under investigation.
Targeted probiotics. Rather than transplanting an entire microbiome, some researchers are testing specific bacterial strains, particularly Lactobacillus species, to prevent UTI recurrence. The evidence is mixed. Some strains show modest benefit, while others perform no better than placebo. The challenge is identifying which specific strains matter.
Mannosides (FimH inhibitors). Washington University researchers developed a molecule that acts as a “decoy” for E. coli’s adhesion proteins, blocking the bacteria from attaching to the bladder wall. In animal studies, mannosides reduced gut E. coli populations without disrupting the broader microbiome. Human trials are ongoing.
Vaginal microbiome restoration. Since bacteria pass through the vaginal area on their way from gut to bladder, some researchers are exploring vaginal microbiome transplants or targeted vaginal probiotics as a complementary strategy, especially for postmenopausal women with atrophic vaginitis.
Phage therapy. Using viruses that specifically target UTI-causing bacteria (bacteriophages) is another active research area. Unlike antibiotics, phages are highly specific and don’t damage beneficial bacteria.
When to See a Doctor
If you experience more than two UTIs in six months or three in a year, talk to your doctor about being evaluated for recurrent UTIs. Standard prevention strategies, including adequate hydration, post-intercourse urination, and possibly cranberry products, should be tried first.
If you’re interested in FMT research, ask your urologist or infectious disease specialist about active clinical trials. You can search for trials at ClinicalTrials.gov using terms like “fecal transplant UTI” or “FMT urinary tract infection.”
Watch for symptoms that need immediate attention: blood in your urine (hematuria), fever with urinary symptoms (which may indicate pyelonephritis), or flank pain, as these suggest the infection may have spread to the kidneys.
For more on prevention strategies you can try now, see our guide on natural ways to prevent recurrent UTIs.
Frequently Asked Questions
What is a fecal transplant and how does it work for UTIs?
A fecal microbiota transplant (FMT) transfers healthy gut bacteria from a screened donor into a patient’s digestive system via colonoscopy, enema, or oral capsules. For UTIs, the goal is to restore a diverse gut microbiome that crowds out UTI-causing bacteria like E. coli before they can migrate to the bladder.
How effective is fecal transplant for preventing recurrent UTIs?
Early studies show promising results. A 2025 Cleveland Clinic study found a 93% reduction in UTIs after fecal transplant 1. A proof-of-concept trial of 22 postmenopausal women showed a 68% reduction 5. These are small studies, though, and larger clinical trials are still needed before this becomes a standard treatment.
Is fecal transplant for UTIs available to patients right now?
Not as a standard treatment. FMT is currently FDA-approved only for recurrent C. difficile infection. For UTIs, it remains investigational and is available only through clinical trials or compassionate-use programs. Ask your doctor about enrolling in active studies if you have refractory recurrent UTIs.
Is fecal transplant safe?
In the UTI studies published so far, no serious adverse events have been reported 6. Common side effects include temporary bloating and digestive discomfort. FMT does carry theoretical risks including transmission of infections and unknown long-term effects. FDA-approved FMT products undergo rigorous donor screening to minimize these risks.
Can fixing your gut bacteria really prevent bladder infections?
Strong evidence supports this connection. A 2022 study in Nature Microbiology showed that women with recurrent UTIs have distinctly depleted gut microbiomes, missing protective bacteria that produce anti-inflammatory compounds 2. A 2019 study proved that UTI-causing bacteria in the bladder are genetically identical to strains in the patient’s gut 3. Restoring gut health may cut off infections at the source.
Summary
The research on fecal transplant for recurrent UTIs is still in its early stages, but the consistency of results across multiple independent studies is hard to ignore. UTI reductions ranging from 68% to 93%, reversal of antibiotic resistance patterns, and significant cost savings all point in the same direction: fixing the gut microbiome may be a more effective long-term strategy than repeated courses of antibiotics.
We’re not at the point of recommending fecal transplant as a UTI treatment. The studies are too small, the follow-up too short, and the regulatory pathway still unfinished. But for the estimated 20-30% of women trapped in the recurrent UTI cycle, especially those dealing with antibiotic-resistant infections, this line of research offers something that has been in short supply: genuine reason for optimism.
If you’re dealing with recurrent UTIs, the practical takeaway right now is this: your gut health matters for your bladder health. While we wait for larger FMT trials, supporting your gut microbiome through diet, targeted probiotics, and avoiding unnecessary antibiotics is a reasonable first step.
References
- Jeong SH, Vasavada SP, Lashner B, Werneburg GT. Fecal Microbiota Transplant Is Associated With Resolution of Recurrent Urinary Tract Infection. Urology. 2025;204:69-75. PubMed
- Worby CJ, Schreiber HL 4th, Straub TJ, et al. Longitudinal multi-omics analyses link gut microbiome dysbiosis with recurrent urinary tract infections in women. Nat Microbiol. 2022;7(5):630-639. PubMed
- Magruder M, Sholi AN, Gong C, et al. Gut uropathogen abundance is a risk factor for development of bacteriuria and urinary tract infection. Nat Commun. 2019;10(1):5521. PubMed
- Choi J, Thanert R, Reske KA, et al. Gut microbiome correlates of recurrent urinary tract infection: a longitudinal, multi-center study. eClinicalMedicine. 2024;71:102490. PubMed
- FMT as treatment for recurrent UTI in postmenopausal women: a proof-of-concept study. Eur J Clin Microbiol Infect Dis. 2025. Springer
- Jeney SES, Lane F, Oliver A, Whiteson K, Dutta S. Fecal Microbiota Transplantation for the Treatment of Refractory Recurrent Urinary Tract Infection. Obstet Gynecol. 2020;136(4):771-773. PMC
- Tariq R, Pardi DS, Tosh PK, Walker RC, Razonable RR, Khanna S. Fecal Microbiota Transplantation for Recurrent Clostridium difficile Infection Reduces Recurrent Urinary Tract Infection Frequency. Clin Infect Dis. 2017;65(10):1745-1747. PubMed
- Bier N, Hanson B, Jiang ZD, DuPont HL, Arias CA, Miller WR. A Case of Successful Treatment of Recurrent UTI by ESBL-Producing Klebsiella pneumoniae Using Oral Lyophilized Fecal Microbiota Transplant. Microb Drug Resist. 2023;29(1):34-38. PubMed
- Hu J, Liu D, Liao G, et al. Fecal microbiota transplantation alleviates immunosuppressant-associated diarrhea and recurrent urinary tract infection in kidney transplant recipients. Gut Pathog. 2025;17(1):28. PubMed
- Baek OD, Hjermitslev CK, Dyreborg L, et al. Early Economic Assessment of Faecal Microbiota Transplantation for Patients with UTIs Caused by Multidrug-Resistant Organisms. Infect Dis Ther. 2023;12(5):1429-1436. PubMed
Frequently Asked Questions
- What is a fecal transplant and how does it work for UTIs?
- A fecal microbiota transplant (FMT) transfers healthy gut bacteria from a screened donor into a patient's digestive system via colonoscopy, enema, or oral capsules. For UTIs, the goal is to restore a diverse gut microbiome that crowds out UTI-causing bacteria like E. coli before they can migrate to the bladder.
- How effective is fecal transplant for preventing recurrent UTIs?
- Early studies show promising results. A 2025 Cleveland Clinic study found a 93% reduction in UTIs after FMT. A proof-of-concept trial of 22 postmenopausal women showed a 68% reduction. However, these are small studies and larger clinical trials are still needed.
- Is fecal transplant for UTIs available to patients right now?
- Not as a standard treatment. FMT is currently FDA-approved only for recurrent C. difficile infection. For UTIs, it remains investigational and is available only through clinical trials or compassionate-use programs. Ask your doctor about enrolling in active studies.
- Is fecal transplant safe?
- In the UTI studies published so far, no serious adverse events have been reported. Common side effects include temporary bloating and digestive discomfort. However, FMT does carry theoretical risks including transmission of infections and unknown long-term effects. FDA-approved FMT products undergo rigorous donor screening.
- Can fixing your gut bacteria really prevent bladder infections?
- Strong evidence supports this connection. A 2022 study in Nature Microbiology showed that women with recurrent UTIs have distinctly depleted gut microbiomes, missing protective bacteria that produce anti-inflammatory compounds. Since UTI-causing E. coli originate in the gut before migrating to the bladder, restoring gut health may cut off infections at the source.
Medical Disclaimer: The information provided is for educational purposes only and should not be considered as medical advice. Always consult with a qualified healthcare professional before making any changes to your diet, supplement regimen, or treatment plan.